Occupational Radiation Safety in Interventional Radiology
Interventional radiology procedures provide less invasive options than traditional surgery. However, they often involve prolonged use of fluoroscopy, exposing medical staff to significant levels of ionizing radiation. The ALARA principle (As Low As Reasonably Achievable) should guide all radiation safety practices. The principle emphasizes minimizing radiation exposure through time, distance, and shielding. Therefore, learning the best approaches to occupational radiation exposure limits is paramount for all professionals working in interventional radiology suites.
Understanding Radiation Exposure
A common misperception in interventional radiology is that the primary source of occupational exposure is direct radiation from the X-ray tube rather than scatter from the patient. In reality, the primary source of radiation exposure to operators and staff is scattered radiation emitted from the patient after the primary X-ray beam interacts with their body. This scattered radiation can reach staff members from various angles, making comprehensive protection essential. Several factors contribute to this misunderstanding:
Visibility of the X-ray Tube
The X-ray tube is a visible, tangible source of radiation, leading to an intuitive but incorrect association with occupational exposure.
Lack of Awareness of Scatter Physics
Staff present during interventional X-ray procedures may not fully appreciate that after absorbing the primary beam, the patient becomes the main source of scattered radiation.
Complex Equipment Geometry
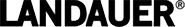
The intensity of scatter can vary depending on the position of the X-ray tube, image receptor, and operator. For example, when the tube is positioned under the table (a typical setup in fluoroscopy), the highest scatter is directed toward the operator's legs. More scatter is directed toward the operator's upper body and eyes when the X-ray tube is positioned over the table.
Operator Positioning
Exposure can be higher on the tube side of the patient than on the image receptor side, especially if the operator stands close to the X-ray tube or the collimator exit port, which are also minor sources of scatter.
Insufficient Training
Inadequate education on radiation safety and scatter patterns perpetuate outdated or incorrect beliefs about exposure sources. Typical occupational skin absorbed dose rates near fixed fluoroscopic equipment in the absence of protective aprons and drapes: (a) over-couch and (b) under-couch X-ray tube. Exposure is typically higher on the tube side than at the image receptor, especially when the operator is close to the patient and the tube.
Personal Protective Equipment
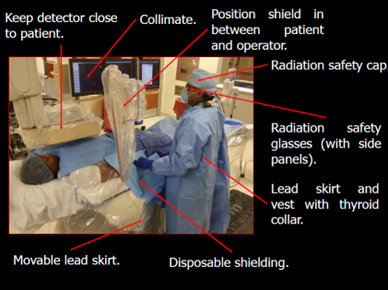
Lead aprons and thyroid shields are essential in the fluoroscopy room, as they can reduce radiation exposure by over 90% when used correctly as personal protective equipment. Ceiling-suspended lead acrylic shields, radiation-attenuating caps, and lead glasses are essential for protecting the head and eyes. Radiation-attenuating gloves offer additional protection for high-exposure areas, such as the hands, which are often closest to the primary beam.
Structural Shielding
Table-mounted shields, ceiling-suspended shields, and mobile barriers offer additional protection by intercepting scattered radiation. Proper positioning of these shields is crucial for maximizing their effectiveness.
Radiation Monitoring

Personal dosimeters (e.g., whole body, collar, and ring) are essential for tracking cumulative radiation exposure. However, real-time dose monitoring systems, such as the RaySafe i3, provide immediate feedback on radiation exposure levels. This real-time information enables staff to adjust their position or techniques during procedures to reduce the dose.
The RaySafe i3 system utilizes color-coded displays to indicate radiation levels, allowing staff to understand their exposure at a glance. This immediate feedback can help users manage radiation exposure by promoting awareness and encouraging behavioral changes (check out this case study). This system is recommended to be used in addition to the passive dosimeter(s) and should not replace passive dosimeter use.
Procedural Techniques for Radiation Safety
Optimal positioning of the X-ray tube and image receptor can significantly reduce scatter radiation. The X-ray tube should be kept below the patient table, and the image receptor should be as close to the patient as possible. Collimation and filtration will reduce the radiation field size and remove low-energy X-rays, respectively, thereby reducing overall radiation exposure. Use last image hold, pulsed fluoroscopy, reduced frame rates (e.g., 7.5 frames per second), and low-dose protocols whenever clinically appropriate.
|
Technique |
Principle of Operation |
Dose Reduction Mechanism |
Main Considerations |
| Pulsed Fluoroscopy | X-ray delivered in pulses, not continuous | Fewer exposures per second | Maintains image quality, best for static/slow-moving targets |
| Reduced Frame Rates | Fewer images per second acquired | Less cumulative exposure over time | It may affect visualization of movement, best for static images |
| Low-Dose Protocols | Adjusts imaging parameters to lower dose | Reduced tube current, voltage, exposure | Tailored to patient/procedure, requires planning |
To enhance radiation safety, it's essential to consider the height of the radiologist and the positioning of the X-ray tube. Adjust the height of the examination table to minimize radiation exposure to the trunk of the body and provide raised platforms for staff members who are shorter in stature. Limit room occupancy to only essential personnel and maintain a safe distance from the X-ray source when not directly involved in the procedure.
Utilize personal protective equipment (PPE) effectively and remember that standing behind another shielded staff member doubles your protection. Ensure that PPE is used correctly and avoid turning unshielded backs towards the X-ray source.
Radioactive Materials
The use of radioactive materials, such as Yttrium-90 TheraSpheres™ and SIR-Spheres® for Selective Internal Radiation Therapy (SIRT), is becoming increasingly common in interventional radiology. These treatments deliver targeted radiation to cancerous tissue but require strict contamination controls. Safety measures include wearing double gloves and shoe covers, scanning staff for radioactivity as they exit the room, and scanning the room for radioactivity before being released for unrestricted use. Consult Nuclear Medicine and radiation safety personnel and consider excluding pregnant staff as per institutional policies.
Education and Training
Ongoing education and training are crucial for maintaining a culture of radiation safety. All staff should receive regular training on radiation protection principles (see our Radiation Protection Program for more info), proper use of protective equipment, and the latest developments in radiation safety techniques. Before handling radioactive materials, the interventional team must be trained to handle contamination and spills. Emergency procedures should be clearly outlined, as some emergency procedures could be different (e.g. call Radiation Safety).
Conclusion
Occupational radiation safety in interventional radiology is a shared responsibility among all parties involved. By understanding the sources of radiation exposure, utilizing appropriate protective equipment and shielding, monitoring radiation doses, employing safe procedural techniques, and participating in ongoing education, all members of the interventional radiology team can work together to minimize radiation risks while providing high-quality patient care.
Remember, radiation is invisible, but its effects are not. Stay vigilant, stay protected, and keep your doses as low as reasonably achievable (ALARA).
Ready to Get Started?
Contact LANDAUER today to learn more about how our radiation safety solutions can help keep your team safe.