Fetal Monitoring: Tracking Radiation Exposure During Pregnancy
Pregnancy is always an emotional and sensitive time. A pregnant medical worker can have a great deal of apprehension regarding the exposure to occupational radiation for the fetus. With the hyper-focus on health and safety at this time, protecting the fetus and eliminating risks are top of mind.
Any employee who works in a medical radiology environment is closely monitored for occupational exposure, but it becomes especially significant when the worker is pregnant. Therefore, it is important to understand how radiation can affect a fetus, how to minimize exposure, and how it’s measured.
In this blog, we discuss topics that an RSO (Radiation Safety Officer) and a pregnant worker should take into consideration:
- Fetal risks of radiation
- Declared Pregnant Worker policy
- Regulatory limit and compliance
- Fetal dosimeter details
- Protective guidance to reduce fetal radiation exposure
Fetal Risks of Radiation
It is important to note that, while low, there are inherent risks with pregnancy, even for healthy people. Although there may not be a personal or family history of reproductive or developmental problems, research shows that for healthy people there is a:
- 3% risk for major congenital abnormalities
- 4% risk of minor congenital abnormalities
- 4% risk of intrauterine growth retardation
- 4 – 10% risk of incidence of genetic abnormalities
- 15% risk of miscarriage
The potential for radiation effects on pregnancy completely depends on the dosage amount received, the time period during which the exposure occurred (was it all in one day or over 9 months?), and the stage of fetal development.
Declared Pregnant Work Policy
There are clear and specific regulations in the national policy regarding pregnancy. The regulations begin with a formal NRC definition (10 CFR 20 .1003) of a Declared Pregnant Worker (DPW): “a DPW is someone who has voluntarily informed the licensee, in writing, of the pregnancy and the estimated date of conception.” The declaration remains in place until the pregnant worker withdraws the notice in writing or is no longer pregnant.
- The declaration is entirely voluntary and must be in writing
- It is up to the employee to decide if the declaration needs to be completed
- The declaration is confidential
- Includes the date of conception
- The NRC regulations do not require medical proof of the pregnancy
- A consultation can be offered by the worker’s facility, and instruction/education given to the employee (10 CFR 19.12)
- US NRC Regulatory Guide 8.13 (most useful to demonstrate compliance) and 8.29
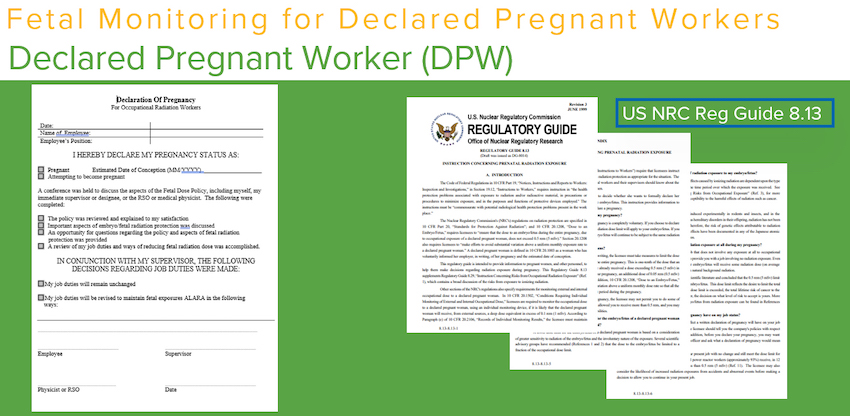
In the image above, you see an example of the Declaration of Pregnancy that a pregnant worker completes. The declaration should include the date of conception, any changes to work duties, and the contact to provide additional information or answer questions the DPW might have. It should also call out who should receive the Declaration of Pregnancy by the name of the individual, the title of a position like RSO, or by a department like HR. The policy should clarify who should be contacted and who will manage the DPW’s work.
- There is no commitment on the part of the licensee to monitor fetal radiation exposure until the DPW completes the written notice.
- When the pregnancy ends, written notice should be given by the DPW to whoever received the initial declaration.
- Many institutions incorporate pregnant worker actions in the annual training. It’s beneficial to have those measures in the education to keep those reminders fresh.
Fetal Radiation Regulatory Limits and Compliance
The NRC reviewed the available literature and concluded that 500 mrem exposure for the gestational period of exposure for fetus provides an adequate margin of protection for the embryo. States have also adopted the limits. While 50 mrem a month is not specifically called out in NRC regulation, the industry standard is to limit the exposure to 500 mrem.
This points to the regulation that requires a licensee to avoid substantial variation above a uniform monthly rate. They must manage the exposure so that it’s about the same every month during the gestational period.
Once the DPW provides notice, the radiation exposure history should be reviewed. Look at the employee’s monthly average to determine if any work duties need to be modified. If exposure is above 50 mrem, some changes must occur in daily work duties. It should be noted that in many cases, workers don’t have to have any changes made to their work duties.
When determining any changes to a DPWs work duties, keep in mind the possibility of:
- Extra shifts
- An increased workload in the future
- Emergency response situations
- On call responsibilities
- Code response
- Challenging cases that could have increased fluoro time
- Nuclear medicine, where there could be increased exposure from the patient.
Work duties may need to be modified initially and monitored throughout the pregnancy to adjust exposure to protect the fetus and maintain a 50 mrem exposure a month or less.
Some institutions will employ a fetal exposure plan in their ALARA program. Adjusted Time, Distance and, Shielding can help reduce fetal exposure. The common exposure in this case is 40 mrem, with a Level 2 investigation initiated if exposure exceeds that amount. LANDAUER offers a notification service triggered at 100 mrem a month or more or a 250 mrem total exposure for the gestational period. The contact for the account will receive the information in the same format they receive other exposure notifications via email or a phone call.
Background and Acceptable Dosage of Radiation
- Doses below 10 rem (100 mSv) should not increase the risk of reproductive effects. (NCRP 174, 2013)
- Fetal exposure limit from occupational sources = 0.5 rem over the gestational period, significantly below the 10 rem level.
- As the pregnancy progresses, the fetus is more sensitive in the early stages of development. However, after 20 weeks, the radiation dosage needed to cause harm to the fetus remains about the same throughout the rest of the pregnancy.
To put this in perspective, using a conservative model, the NCRP has concluded that for a fetus exposed to 50 mrem (0.050 rem) in utero, the probability of live birth with no malformations or cancer is reduced from 95.93% to 95.928%
Fetal Dosimeters
Once you have the written DPW notice, you can contact LANDAUER by calling or logging in online through the MyLDR portal to provide the conception and declaration dates and order a fetal dosimeter. It is the same Luxel dosimeter used for full-body or area monitoring. However, it will have a baby icon seen on the front to give you an easy visual way to discern between the fetal monitor and a regular dosimeter. It will also say ‘Fetal” on the back. All fetal dosimeters will always be exchanged on a monthly frequency, independent of the exchange frequency of the regular full-body dosimeters exchange. If an institution has a spare dosimeter, it can be used as a fetal monitor. Just make sure you notify LANDAUER that the spare dosimeter is being substituted as a fetal monitor for that individual.
 The fetal dosimeter is worn at the waist, and if the DPW is wearing PPE, it should be worn underneath lead shielding to reflect the exposure accurately. It is worn in addition to the whole-body dosimeter. Always be diligent in making sure the fetal monitor is worn in the correct location. This can be challenging as the body expands but the DPW should do their best to position the dosimeter at the area defined as ‘waist’ LANDAUER has experience looking at reports that show exposure was greater in the fetal area than the collar location which immediately indicates the dosimeters were swapped. Reinforce with DPW that the fetal dosimeter is always worn in the correct location.
The fetal dosimeter is worn at the waist, and if the DPW is wearing PPE, it should be worn underneath lead shielding to reflect the exposure accurately. It is worn in addition to the whole-body dosimeter. Always be diligent in making sure the fetal monitor is worn in the correct location. This can be challenging as the body expands but the DPW should do their best to position the dosimeter at the area defined as ‘waist’ LANDAUER has experience looking at reports that show exposure was greater in the fetal area than the collar location which immediately indicates the dosimeters were swapped. Reinforce with DPW that the fetal dosimeter is always worn in the correct location.
Luxel dosimeters are angle dependent and should always be worn facing the radiation source. We strongly discourage wearing them on a lanyard or ID clip because they might flip backward. The fetal dosimeter is worn under shielding and for occupational radiation exposure only. If the DPW is getting radiation for personal reasons as a patient (dental work, etc.), she should not wear the fetal dosimeter during those procedures. While the personal medical imaging doesn’t necessarily pertain to occupational exposure to the fetus, it is always good for the DPW to have a discussion with the medical provider to understand the exposure from the procedure and confirm the dose amount is safe for the fetus.
Reporting Fetal Dose
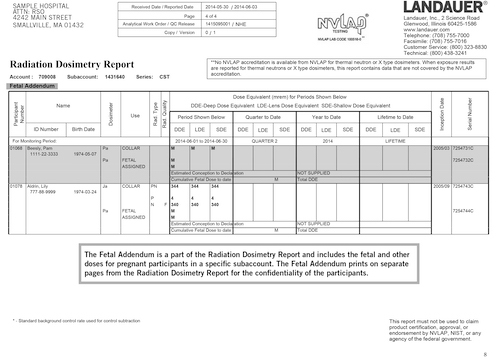 To the right is an example of a Fetal Addendum report from the MyLDR portal. On the left, under the title, Radiation Dosimetry Report, is highlighted “Fetal Addendum”. It helps identify that these are fetal exposures. While they are provided as a separate file, they will also be included in the standard dosimetry report for the relevant time periods. The report shows the participant’s exposure from a collar dosimeter and then the fetal dosimeter. Finally, you can see the relevant dates and the cumulative exposure for the sum total of the fetal exposure for that individual.
To the right is an example of a Fetal Addendum report from the MyLDR portal. On the left, under the title, Radiation Dosimetry Report, is highlighted “Fetal Addendum”. It helps identify that these are fetal exposures. While they are provided as a separate file, they will also be included in the standard dosimetry report for the relevant time periods. The report shows the participant’s exposure from a collar dosimeter and then the fetal dosimeter. Finally, you can see the relevant dates and the cumulative exposure for the sum total of the fetal exposure for that individual.
A featured Fetal Monitoring Report is also available if requested. It is a separate and efficient snapshot of the dose exposure for all the DPW participants for the past year. The results stay on the report for a rolling 12 months so, any worker who was/is pregnant in the past calendar year, will appear on this report (even if they are not currently pregnant).
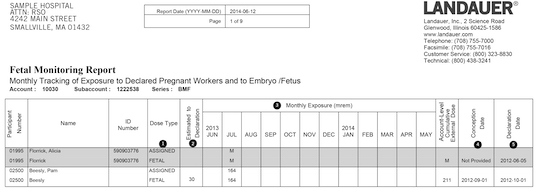 There are several key pieces of information provided. Under the dot marked #1 in the column, Dose Type, the data tells you if the dose recorded is from a fetal dosimeter or if it was assigned from a whole-body dosimeter. The dot marked #2 is the dose between the conception date and the declaration date. The information is provided by the customer to LANDAUER and is done when the fetal monitor is ordered to complete the dose of record. Dot #3 shows the monthly exposure. The columns on the left marked #4 and, #5 show the total fetal dose summed up for each participant.
There are several key pieces of information provided. Under the dot marked #1 in the column, Dose Type, the data tells you if the dose recorded is from a fetal dosimeter or if it was assigned from a whole-body dosimeter. The dot marked #2 is the dose between the conception date and the declaration date. The information is provided by the customer to LANDAUER and is done when the fetal monitor is ordered to complete the dose of record. Dot #3 shows the monthly exposure. The columns on the left marked #4 and, #5 show the total fetal dose summed up for each participant.
Terminating Fetal Dose Monitoring
The institution must complete two steps to terminate a fetal dosimeter within the LANDAUER system. The first step is to call or log in to MyLDR and turn in the fetal dosimeter. The second step is to provide the pregnancy end date. It’s the last day of fetal monitoring. It can be the delivery date or the date the worker left for maternity leave, etc. Essentially, it’s the last day of fetal monitoring. Suppose the fetal monitor is not returned for a wear period or the pregnancy end date is not given. In that case, LANDAUER will assign the fetal dose from the participant's whole-body dosimeter. It is vital that the two steps be taken at the end of the pregnancy. The declaration of a DPW is in effect until the pregnant worker withdraws the declaration or is no longer pregnant.
Protective Guidance for Fetal Exposure
It is wise to revisit the three principles of ALARA - Time, Distance and, Shielding – which can help reduce fetal exposure. Initially, you may think of shielding PPE and, indeed those are critical, but this is the time to consider exposure as it relates to ALARA and pay attention to less time, more distance, etc.
- Time: arrange to have less time exposed to the point source.
- Distance: move farther away. The greater the distance, the less exposure to the point source. Doubling the space between the worker and the point source can reduce the exposure to one-quarter of what it was at the original distance.
- We do not recommend wearing two aprons when wearing one and focusing on time and distance seems to be a better balance of the ALARA concepts.
Pregnancy and Nuclear Medicine
It is strongly recommended that the DPW avoid 131-I therapy. They involve high activity, and the I131 carries an energetic gamma. In addition, the radioiodine easily crosses the placenta, and the fetal thyroid will accumulate this radioiodine making it an internal and external exposure hazard. Using L-blocks and syringe shields will help reduce exposure. Finally, be mindful of the distance from injected patients; it could be a time of very close proximity to the source and, keeping distance can help reduce DPWs’ exposure.
With fluoroscopy, it might be a good idea to consider a wraparound shield PPE for the DPW. Wraparound shield offers advantages over heavy lead aprons:
- 360° coverage
- Evenly distributed weight makes it more comfortable
- Wear the correct size PPE, with no gaping armpits etc.
- Lighter weight lead equivalent options are available
- Should have the 0.5 mm lead equivalent required by the regulations
- Can be significantly lighter than lead
- Environmentally friendly
- Can be expensive
Additional Points of Interest
Accounting for the time between a conception date and the written date of declaration can be done by contacting LANDAUER and providing the estimated dose for that time period. That way, there is a comprehensive record of total fetal exposure.
If an employee expresses concern that the Declaration of Pregnancy might affect their job status, it is up to the facility to review the exposure history and current work duties. The issue could also be considered before the pregnancy is declared and any potential changes discussed. Then the institution can let the pregnant worker decide whether to file a Declaration.
The choice to provide a written declaration is entirely up to the individual and can be revoked whenever she wants. However, the statement to revoke should be in writing, fetal monitoring ends, and the licensee is not required to maintain the lower fetal dose exposure.
The question of automatically providing fetal monitors to all DPW in a facility regardless of their work role or job title (administrative staff, cleaning staff, etc.) does come up. However, it is a decision entirely left up to the facility and what it chooses to write into the policy.
Sometimes a worker may share that they are trying to get pregnant and may inquire about getting a fetal dosimeter. However, until a Declaration of Pregnancy is provided, the licensee is not required to provide a fetal dosimeter. The facility could suggest that they wear a chest or waist dosimeter in the location a fetal dosimeter would be worn. It could be an opportunity to collect fetal exposure data between conception and a written declaration. It’s also a good time to reinforce time, distance and, shielding practices.
 Many other radiation sources are constant in our daily lives, like microwaves, cell phones, computers, power lines, airport screening, etc. Fetal exposure to non-ionizing radiation sources is not the responsibility of the occupational institution/licensee, nor does the DPW policy cover these sources. However, a DPW may ask and the licensee can assure her that she is safe. The risk of these sources on a fetus have been studied extensively by two national committees who have reviewed the data, published books, and concluded that the reproductive risk is minimal if it even exists.
Many other radiation sources are constant in our daily lives, like microwaves, cell phones, computers, power lines, airport screening, etc. Fetal exposure to non-ionizing radiation sources is not the responsibility of the occupational institution/licensee, nor does the DPW policy cover these sources. However, a DPW may ask and the licensee can assure her that she is safe. The risk of these sources on a fetus have been studied extensively by two national committees who have reviewed the data, published books, and concluded that the reproductive risk is minimal if it even exists.
National and state radiation regulatory agencies provide excellent guidelines for a licensee to follow to provide the safest possible work environment for a pregnant worker. Knowing your institution’s policies and following the tips outlined above will ensure that the pregnancy will be monitored and the fetus kept safe from any over-exposure to occupational radiation.