Radiation Equipment Inspection: Readiness Checklist
Radiation Equipment Inspection
Radiation equipment inspections focus on patient safety, occupational safety (e.g., occupational radiation exposure), quality patient care, and infection control. Radiation exposure (i.e., dose) occurs in facilities using sources of ionizing radiation including hospitals, imaging and therapy centers, research facilities, health clinics, laboratories, chiropractic offices, dental clinics, and animal hospitals or veterinary clinics. Sources of ionizing radiation are also used in industrial operations, aerospace operations, manufacturing, and mining. Depending on the use, the inspectors will change. Occupational safety is a key, common feature wherever hazardous materials are used. This article focuses on the use of radiation sources in medicine (except radiation therapy), dentistry, and veterinary practice.
Regulations
Nuclear Regulatory Commission (NRC) or Agreement State regulations govern the use of radioactive materials (Title 10, Code of Federal Regulations). Agreement States have agreed with the NRC to license and inspect locations and sources of radioactive materials within their borders. The states regulate standards for machine-produced sources of ionizing radiation. State standards can be more stringent than federal regulations. In addition to federal and  state regulations, hospitals and health clinics are expected to implement best practices to reduce risks to staff and patients, continually improve the quality of patient care, and protect the environment. Various accreditation agencies (e.g., The Joint Commission) inspect and accredit hospitals, medical offices, nursing homes, laboratories, and ambulatory health clinics to assess life safety and best health and environmental practices. While inspections and accreditation are voluntary, Medicare and third-party reimbursement for patient care are tied to Joint Commission accreditation.
state regulations, hospitals and health clinics are expected to implement best practices to reduce risks to staff and patients, continually improve the quality of patient care, and protect the environment. Various accreditation agencies (e.g., The Joint Commission) inspect and accredit hospitals, medical offices, nursing homes, laboratories, and ambulatory health clinics to assess life safety and best health and environmental practices. While inspections and accreditation are voluntary, Medicare and third-party reimbursement for patient care are tied to Joint Commission accreditation.
The Radiation Safety Program
An effective radiation safety program reduces risks (e.g., misdiagnosis, adverse medical events, and public embarrassment). The efforts required are justified by positive radiation equipment inspection results that convince facility staff, facility leaders, and the public that quality images are being produced while maintaining radiation dose As Low As Reasonably Achievable (ALARA). Effective radiation safety policies or programs include but are not limited to the following:
Radiation Safety/ALARA program
- Management has committed in writing to support the Radiation Safety/ALARA program
- The Individual Responsible for Radiation Protection (IRRP) or the Radiation Safety Officer (RSO) is appointed by management to ensure compliance with the Radiation Safety Program
- The Radiation Safety Program is reviewed at least annually for accuracy and regulatory compliance by the IRRP or the RSO
Occupational/Public Dose
- Radiation workers are provided and wear dosimeters from an accredited laboratory (e.g., NVLAP) while working with sources of ionizing radiation
- Dosimeters are stored in a designated low background radiation area when not in use
- Occupational dose results are reviewed periodically (e.g., quarterly) by the IRRP or RSO and provided to radiation workers at least annually, consistent with the Radiation Safety Program
- Radiation dose is assessed in areas adjacent to radioactive materials use areas (e.g., Area Monitor dosimeters) and demonstrates that public dose does not exceed 1 millisievert (100 mrem) per year and 0.02 millisieverts (2 mrem) in any one hour
NOTE: The dose results from personal and area monitor dosimeters, used or placed in areas where the radiation dose is assumed to be low, can demonstrate that it is low.
Training
- Radiation workers and those who frequent ionizing radiation use or storage areas receive periodic (e.g., annual) safety training commensurate with the risks to include: the risks and biological effects of radiation, the effects on the growing embryo-fetus, dose limits, the use of dosimeters, principles/practices to maintain radiation dose ALARA (e.g., time, distance, and shielding), local policies/procedures, worker’s rights/obligations, and emergency procedures. If radioactive materials are used, the training includes the safe preparation and handling of radioactive materials/packages, applicable license/authorization limits and requirements, access control, and radioactive survey/spill procedures
- Staff members date and sign a training roster that describes the content of the annual radiation safety training they received. Since local radiation safety policies/procedures cannot be discussed in their entirety during annual training, consider having staff sign a cover letter attached to a bound copy of these policies/procedures indicating they have read and understood them
Image Quality Control Program
- Radiation workers are registered and/or licensed to meet federal and state requirements to use sources of ionizing radiation
- Image Quality Control Program records are maintained to include evidence of staff and patient dose and the calibration and periodic inspection of X-ray equipment, and gamma cameras
- Radiation dose should not exceed diagnostic reference levels for a given study
- Repeat or retake logs are maintained and reviewed that include the reason, room number, date, and technologist
Facilities/PPE
 Appropriate warning signs are posted at the entrances to ionizing radiation use areas (e.g., “Caution X-ray,” “Caution Radioactive Materials,” “Caution Radiation Area,” “Caution High Radiation Area,” and “If You Think You May Be Pregnant, Inform the Technologist”)
Appropriate warning signs are posted at the entrances to ionizing radiation use areas (e.g., “Caution X-ray,” “Caution Radioactive Materials,” “Caution Radiation Area,” “Caution High Radiation Area,” and “If You Think You May Be Pregnant, Inform the Technologist”)- Warning labels are affixed to the X-ray control panel stating, “Warning: This x-ray unit may be dangerous to patient and operator unless safe exposure factors, operating instructions and maintenance schedules are observed” or similar wording as required by state regulations
- A label is affixed to the X-ray tube housing stating “This Product Complies With DHHS Requirements of 21 CFR, Subchapter J”
- Access to X-ray systems and radioactive materials is controlled to prevent unauthorized use or theft
- Lead or lead equivalent aprons and other protective devices are available for staff and patient use consistent with the Radiation Safety Program
- Appropriate personal protective equipment is worn when performing portable radiography and handling radioactive materials
- Lead aprons and other lead protective devices are periodically inspected (e.g., annually) for cleanliness and defects (integrity) consistent with the Radiation Safety Program
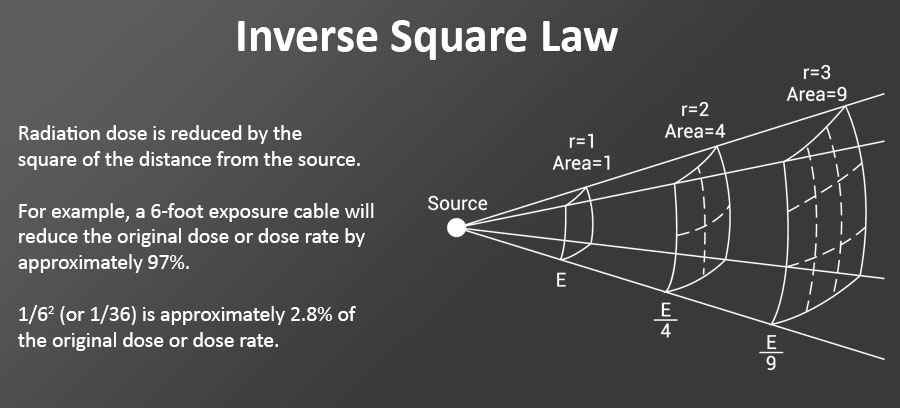
- X-ray operators can energize the X-ray systems from behind a leaded control booth or for mobile systems, from the end of a 6-foot exposure cable while wearing a lead apron
- The operator can see the patient while energizing the X-ray system (minimize retakes)
- Image phosphors and imagers (computed radiography) are cleaned following the manufacturer’s instructions and checked for scratches, chips, and exposure uniformity
- Radiolucent positioning devices, slings, sandbags, restraints, or sedatives are available in veterinary practice to facilitate radiography while minimizing human exposure
- Veterinarians or staff technologists should maintain a log with exposure date, exposure techniques, machine operator, type/identity of the animal, and name of individuals holding the animal during X-ray procedures
Radioactive Materials
- Dose calibrators used to measure radiopharmaceuticals before patient use are periodically calibrated according to the manufacturer’s specifications or nationally recognized standards and your state's regulations
- Radiopharmaceuticals are effectively measured/labeled to avoid medical events
- If radionuclide generators are used (i.e., Mo-99/Tc-99m or Sr-82/Rb-82), Mo-99 concentration is measured before each elute or Sr-82 and Sr-85 concentrations are measured before the first patient use of the day.
- Radiation detection and survey equipment are calibrated at least annually
- Radioactive materials are ordered, received, used, and disposed of consistent with the facility license/authorization for their use
- Prescriptions for the therapeutic use of radioactive materials or any use of radioiodine are reviewed periodically to ensure the use was consistent with the prescription and in compliance with the quality management program
- Radioactive packages are received and opened appropriately and within 3 hours of receipt or the start of the next duty day if received after duty hours
Specific credential requirements apply to radiologists, technologists, and medical physicists for advanced imaging modalities (e.g., Radiation Therapy, Nuclear Medicine, Computed Tomography, and Mammography). Regulatory requirements for mammography facilities and providers are specified in the Mammography Quality Standards Act (MQSA).
The Image Quality Control Program (IQCP)
The use of modern, digital X-ray equipment with automatic exposure control (AEC) often leads us to believe that the dose to our patients and potentially to ourselves is low. However, image processors are designed to adjust over-exposed images to make them appear diagnostic. As part of your image quality control program, medical physicists should periodically calibrate the AEC to ensure that quality images are being produced with minimal patient dose. The RSO or the quality control technologist should be able to explain to inspectors how the dose to patients is maintained ALARA (e.g., Image Wisely / Image Gently). Inspections (i.e., at least annual) by biomedical equipment repair personnel and health or medical physicists should be reviewed for trends and to ensure identified deficiencies were corrected. Repeat/retake exams should be included as part of the IQCP. A review of repeat exams can reveal equipment problems or the need for remedial training.
Preparation for Radiation Equipment Inspections – an ongoing part of doing business
The IRRP or RSO needs to be vigilant and perform annual and periodic, unannounced inspections while reinforcing best radiation safety practices. This will produce greater risk awareness, reduce serious incidents, lower radiation dose, improve the quality of patient care, and the overall radiation safety program (i.e., foster a radiation safety culture).
If you want to know more about the inspection of diagnostic imaging facilities, you can visit The Joint Commission’s website and review their Imaging Checklist or the American College of Radiology and the American Association of Physicists in Medicine Radiation Safety Officer Resources document.